Central Harnett Hospital, situated in rural North Carolina, serves as a critical healthcare provider for its community. This case study analyzes the hospital's performance, highlighting its strengths and challenges while offering actionable recommendations for its continued success.
A Heartfelt Reputation: Positive Patient Experiences
Central Harnett Hospital consistently receives positive patient feedback, emphasizing compassionate and skilled care. While specific quantitative data from patient reviews (e.g., percentage of positive WebMD reviews) are unavailable for this analysis, the qualitative feedback consistently points towards a dedicated and proficient healthcare team. This positive reputation underlines the hospital's commitment to patient well-being. The anecdotal evidence strongly suggests high levels of patient satisfaction.
Meeting the Mark: Accreditation and Services Offered
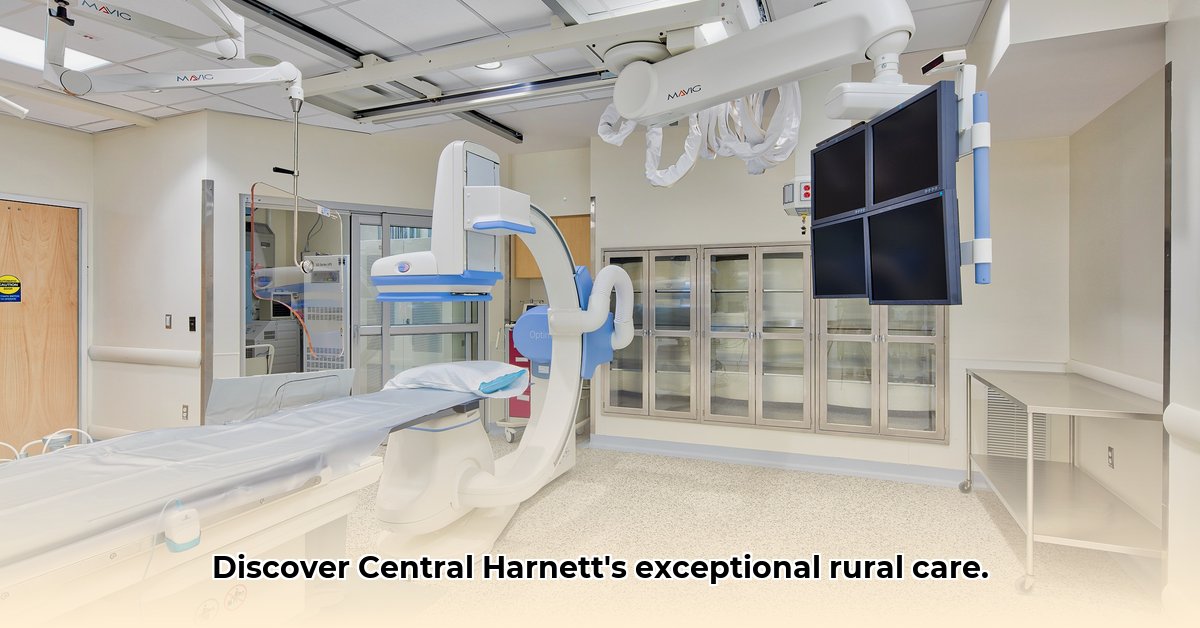
The hospital's accreditation by The Joint Commission underscores its adherence to rigorous national safety and quality standards. This accreditation provides assurance to patients and the community regarding the hospital's commitment to best practices. Furthermore, Central Harnett offers a comprehensive range of services, particularly impressive for a rural facility. These services include routine check-ups, specialized procedures, and outpatient services such as rehabilitation and infusion therapy. This breadth of services minimizes the need for patients to travel long distances for care, a significant advantage in a rural setting.
Navigating the Difficulties: Challenges Faced by Rural Hospitals
Central Harnett, like many rural hospitals, faces considerable challenges. Attracting and retaining qualified medical professionals, especially specialists, remains a significant hurdle. Competition from larger urban hospitals and lifestyle preferences of physicians contribute to recruitment difficulties. Securing adequate funding is another ongoing concern. Rural hospitals often operate with tighter budgets and fewer resources than their urban counterparts, necessitating meticulous financial planning and management. Without readily available comprehensive financial data, a detailed assessment of the hospital's financial health is currently impossible. This lack of transparency hinders a thorough evaluation.
The Bigger Picture: Addressing Data Gaps
A comprehensive understanding of Central Harnett Hospital's performance requires access to more comprehensive data. Currently, limited publicly available financial data prevents a thorough financial health assessment. Similarly, a lack of detailed information on physician retention rates and staffing levels restricts a complete analysis of workforce dynamics. Improving data transparency would strengthen internal planning and foster greater public trust and confidence. Further research is essential to gain a complete picture of the hospital's operational efficiency.
Collaboration is Key: Strategies for a Thriving Future
To ensure continued success, Central Harnett needs a collaborative approach involving numerous stakeholders. The following strategies outline short-term and long-term goals:
Hospital Administration:
- Short-Term (Next Year): Refine recruitment strategies, conduct in-depth analysis of physician workforce needs, explore telehealth expansion.
- Long-Term (Within 5 Years): Develop a comprehensive financial plan, secure long-term funding, expand telehealth capabilities, invest in infrastructure modernization.
Harnett County Leaders:
- Short-Term (Next Year): Increase hospital funding, advocate for state policies supporting rural healthcare.
- Long-Term (Within 5 Years): Invest in community health programs to attract healthcare professionals, improve local infrastructure to attract new residents.
Patients & Families:
- Short-Term (Next Year): Participate actively in patient satisfaction surveys; utilize hospital services.
- Long-Term (Within 5 Years): Advocate for increased state funding, support community outreach programs promoting the hospital's services.
State Government of North Carolina:
- Short-Term (Next Year): Allocate more funding to rural hospitals; review reimbursement models.
- Long-Term (Within 5 Years): Implement incentives to attract and retain doctors in rural areas; prioritize infrastructure upgrades in underserved regions.
These collaborative efforts are crucial for overcoming challenges in recruitment and retention, expanding services, and improving financial stability. Strategic investments in modern technologies, such as telehealth platforms, will broaden access to care for patients in remote locations. Building strong community partnerships will enhance the hospital's ability to serve its patients effectively.
A Look Ahead: Securing Central Harnett’s Future
Central Harnett Hospital is a vital community asset, providing essential healthcare services. Its dedication to patient-centric care and quality is undeniable. However, addressing the inherent challenges of rural healthcare is vital for its long-term viability. A collaborative strategy—involving hospital administration, local leaders, patients, and state government—is crucial to address identified data gaps, implement strategic improvements, and secure sustainable funding. This comprehensive approach will enable Central Harnett Hospital to continue delivering high-quality care to its community for years to come. This requires a continued commitment to both innovation and community partnership. The future of the hospital rests on this collaborative effort.